(DITI and thermogram are used interchangeably )
What is digital infrared thermal imaging?
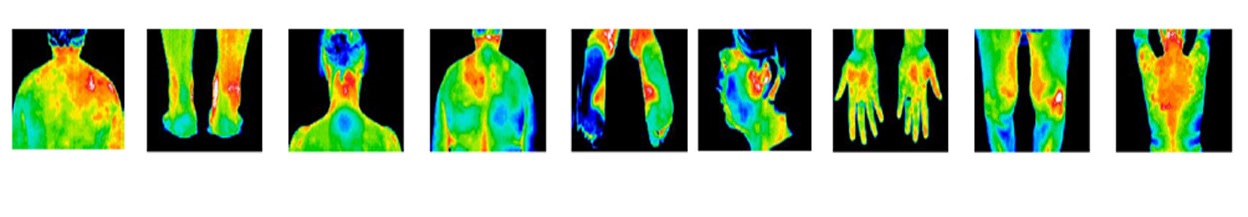
Digital Infrared Thermal Imaging (DITI), is a FDA approved method of measuring patterns of heat emitted from the body. A scan of the body (or particular area) is taken and read by a medical doctor. If any part of the body appears too hot or too cold, the doctor will make a recommendation on how to further check the questionable area using other diagnostic tools.
People can image their entire body to look for any potential issues such as cancer or diabetes. The most popular imaging, though, is the breast area. DITI detects angiogenesis which is the growth of new blood vessels. These new blood vessels feed a tumor and they show up as higher temperature in breast tissue.
What is the difference between DITI and a mammogram?
First, these are two entirely different methods of screening for breast cancer and DITI does not replace mammograms. Mammograms detect structure or anatomy such as a tumor; DITI detects a process or physiology like inflammation or angiogenesis. However it is an excellent adjunct to regular testing (see NIH study).
Second, mammograms use radiation and compression; DITI uses neither – so there is no damage to fragile, cellular DNA and there is no risk from radiation (and even though mammograms use low radiation, THERE IS NO SAFE LOW RADIATION). For women with BRCA 1 or 2, please click on “Research” and then “Clinical Studies.”
Third, DITI views a larger area (all the way up parallel to and under the arm pit) which is one of the reasons why they have a better detection rate.
Fourth and most importantly, because DITI detects the growth of new blood cells, they detect cancerous conditions in the breast up to 8 years before a mammogram can detect a tumor. So since no one knows how to prevent cancer, early detection seems to be your best chance for overcoming this dreaded disease.
How accurate is each method?
For women over 50, mammograms are accurate 80% – 84% of the time. For women under 50, this accuracy drops to 60% because of the density of their breasts. DITI misses non-growing and/or fully encapsulated tumors. For more information on these conditions, please click on Research and under articles “Why Thermograms are important for Mammography”.
For early detection, which method is better?
| Women between the ages of 30 to 50 have denser breast tissue which makes it more difficult for mammograms to pick up any suspicious lesions. Also, cancer for these women is the more aggressive type. This chart shows the growth rate of cancerous cells. In women under 50, the average doubling time is 80 days; in women over 50, it is around 160 days. So because a younger woman’s cancer grows more quickly, early detection is of utmost importance and thermograms are particularly suited to do this. (See Chart on Home Page) |
Why haven’t I heard more about thermograms?
Thermograms are not covered by insurance. When thermograms first came on the scene in the 1980’s, they were used mostly to verify injury on insurance claims. The insurance industry lobbied successfully to have them not be covered.
Second, again when thermograms first came out, they were showing abnormalities which the mammograms could not detect. These findings were called false positives and placed thermal imaging under suspicion. However, in re-call studies, a large percentage of these women developed breast cancer in the exact location of the abnormal false positive.
So today, doctors may be unaware of the real history and that thermograms got FDA approved for breast cancer screening in 1982. Also, some doctors fear that if they do not recommend mammograms as the gold standard of breast cancer detection, they will have their licenses revoked.
Could you describe the procedure?
A patient undresses from the waist up and is given a paper gown or cape to put on. She then fills out a brief questionnaire and Rachel addresses any concerns the patient might have. This is a very important time because during this conversation, the body has time to acclimate to the room temperature of about 72 degrees. The camera is then placed slightly less than 3 feet away from the patient. The patient then sits for about 5 seconds for each of 6 posses. There’s a front view, 2 sides, 2 diagonal and an optional back or posterior view.
The scans are electronically transmitted directly to a specially trained and board certified MD. This doctor then reads the scan, writes the report, and sends it back to Rachel – all within 24 hours. Rachel then mails out 2 copies for the client who can then take a copy to her doctor.
Have there been clinical tests done on thermal imaging?
Absolutely. Over 800 peer reviewed studies on Breast Thermography have been conducted. Well over 300,000 women have been studied. And some of the studies have followed patients up to 12 years. These trials have shown the many benefits of thermal imaging including its ability to detect the first signs of cancer up to 8 years before any other procedure can detect a cancer.
Who certifies your thermographer?
Thermography technicians are trained and certified by an accredited medical association. Our thermographer, Rachel, has been imaging people for over 10 years.
What if the thermogram finds something suspicious? What do I do?
If the thermogram says the clinical correlation is urgent, you need to take the report to your doctor so he or she can do further testing. If your doctor does nothing, you need to let us know. We will contact the doctor directly to give further clarification. Let’s be very clear about this: thermography is a scientifically viable, FDA approved screening tool and if the scans detect warning signs, these signs should not be ignored.
How often do I need to do thermal imaging?
The first year you need to do 2 – three months apart. Everyone has their own unique thermal pattern – just like a fingerprint. The two series of scans establish a baseline – from that baseline, a yearly thermogram is recommended.
What do thermograms cost?
Initial and Annual Thermal Scanning: $190
3 month follow-up: $150
One Region of Interest: $170
2 Regions of Interest: $250
Half Body: $280
Full Body (includes any special study): $380
Includes 1 copy of a full report, including images, by a MD who is board certified as a Thermologist. The Report will be emailed with password protection. Any Report that is mailed will be $5.00 extra.
How often does our thermographer come to Kure Spa & Wellness Center?
Rachel is with us once a month. Usually it s the last Tuesday of every month.